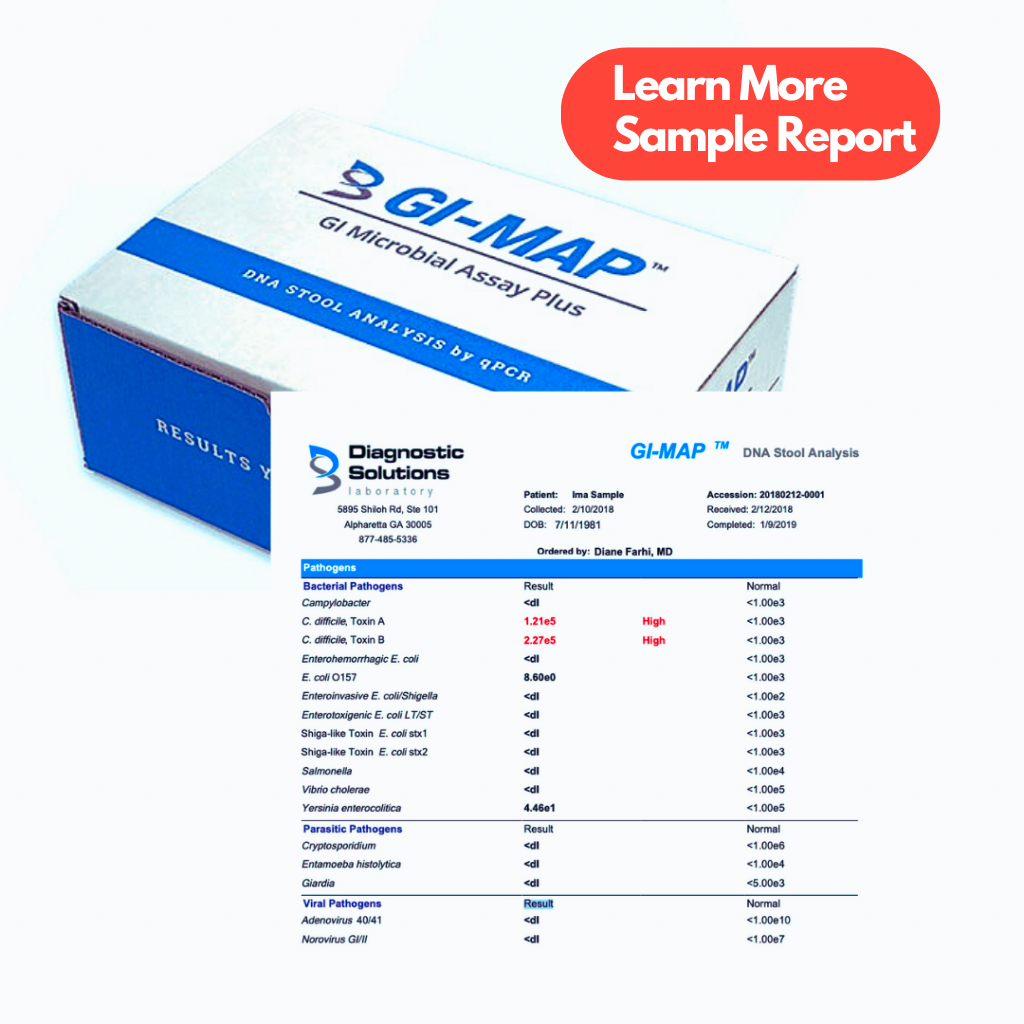
GI-MAP Stool Test | Diagnostic Solutions
The GI-MAP home stool test, developed by Diagnostic Solutions Laboratory, utilizes cutting-edge DNA technology to pinpoint the condition of your gut microbiome with remarkable precision.
This advanced approach bypasses the limitations of traditional stool tests, which often miss crucial data due to bacteria dying off before they can be tested. If you have watched the documentary “Hack Your Health: The Secrets of Your Gut,” this is your microbiome test.
It’s not just about the beneficial gut flora, the GI-MAP stool test goes further to identify and analyze harmful bacteria, viruses, parasites, and fungi, which can disrupt the delicate balance of your gut’s good microbiome.
Not only does the GI-Map reveal harmful bacteria, but (as an add-on) it also tests for their genetic makeup to understand their resistance to antibiotics (see the bottom table).
This critical information helps you and your healthcare provider have more treatment options, ensuring that any interventions, medical or nutritional, are as effective as possible in supporting your gut health.
We also offer a one-on-one GI Map results review service so that you can understand your test results and have a more productive conversation with your treating healthcare practitioner.
How Do I Interpret the GI Map Microbiome Stool Test Results?
The GI-MAP microbiome stool test provides a detailed look into your gut health, showing gut bacteria imbalances and infections that could cause long-term health effects.
Interpretation of the GI Map Stool test should be done by a qualified healthcare practitioner. However, here are the 9 key categories the test assesses, what to watch for in each, and an interpretation video to break down the GI Map test in detail.
- Pathogens: Look for high levels of bacteria, viruses, or parasites. Elevated markers indicate potential infections.
- Beneficial Bacteria: Check for optimal levels of good bacteria like Lactobacillus, Bifidobacterium, and Akkermansia. Low levels may suggest a need for personalized probiotic support.
- Opportunistic Bacteria: Elevated levels can signal gut dysbiosis. These bacteria thrive when the gut environment is imbalanced.
- Fungal/Yeast Overgrowth: High Candida levels can lead to symptoms like bloating and fatigue. Addressing this may require dietary changes and antifungals.
- Digestive Enzymes: Low elastase-1 levels could indicate pancreatic insufficiency. Consider digestive enzyme supplementation if levels are low.
- Inflammation Markers: High calprotectin or lactoferrin levels suggest gut inflammation. This might be linked to conditions like Inflammatory Bowel Disease (IBD), brain fog, bloating, and depression.
- Immune Function: Secretory IgA reflects gut immune health. Low levels may indicate weakened gut immunity which could also lead to higher inflammation.
- Fat Malabsorption: Elevated steatocrit levels can suggest issues with fat digestion. Dietary adjustments or enzyme support may be needed.
- H. Pylori: Positive results could indicate a Helicobacter pylori infection, which may require treatment to prevent ulcers and improve stomach acid production.
What’s In Your GI-Map Stool Test: The Details
Microbiome Flora (Good Bacteria)
- Bacteroides fragilis: Plays a key role in developing a robust immune system and preventing harmful inflammation in the digestive tract.
- Bifidobacterium: Important for breaking down food, fighting harmful bacteria, and producing essential vitamins (B1, B2, B3, B6, B9 (folic acid), B12, vitamin K) that support proper function of all cells.
- Enterococcus: Contributes to a healthy gut environment and assists in the digestion process, converting food into energy.
- Escherichia (E. Coli): Certain strains can be harmful, while others are helpful, maintaining the integrity of the intestinal barrier and preventing infections.
- Lactobacillus: Needed to maintain a healthy balance of gut flora, warding off pathogens, and aiding in digestion.
- Akkermansia mucinophila: Helps reinforce the mucous layer in the gut, acting as a protective barrier and playing a role in metabolic processes. Imbalances of Akkermansia can lead to unexplained weight gain.
- Clostridia: Involved in the synthesis of important nutrients and the maintenance of a healthy and balanced gut microbiota.
- Faecalibacterium prausnitzii: Has anti-inflammatory properties that are crucial for the health of the gut lining and preventing disorders like Irritable Bowel Syndrome (IBS).
- Roseburia: Known to produce butyrate, a short-chain fatty acid that fuels colon cells and supports a healthy colon.
Bad Bacteria
- Campylobacter: Causes foodborne illness with symptoms like fever, diarrhea, and abdominal pain, often from undercooked poultry.
- Clostridium difficile, Toxin A: Releases toxins that damage the intestines, leading to severe diarrhea and colitis, often after antibiotic use.
- Clostridium difficile, Toxin B: Similar to Toxin A, it also causes severe intestinal conditions and is associated with hospital-acquired infections.
- E. coli: Some strains like O157:H7 can cause severe stomach cramps, bloody diarrhea, and vomiting. There are other strains that are healthy for us.
- Enterotoxigenic E. coli LT: Produces a toxin causing watery diarrhea, especially in children in developing countries.
- Enterotoxigenic E. coli ST: Produces a toxin and is a common cause of traveler’s diarrhea.
- Shiga-like Toxin E. Coli stx1: Produces a toxin causing hemorrhagic colitis and can lead to a severe condition known as hemolytic uremic syndrome.
- Shiga-like Toxin E. Coli stx2: Similar to stx1, but often associated with more severe outcomes and complications.
- Shigella: Can cause symptoms like fever, stomach pain, and diarrhea, which can be bloody.
- Salmonella: Can produce symptoms like diarrhea, bloating, fever, and abdominal cramps, often from contaminated food.
- Vibrio cholera: Responsible for cholera, which causes severe watery diarrhea and can lead to dehydration and death if untreated.
- Yersinia enterocolitica: Often leads to yersiniosis, causing symptoms like diarrhea, fever, and abdominal pain, sometimes leading to severe complications.
Viruses
- Adenovirus 40/41: Commonly causes diarrhea in children and can also lead to respiratory infections.
- Norovirus GI: A leading cause of gastroenteritis, with symptoms including diarrhea, vomiting, nausea, and stomach pain.
- Norovirus GII: Similar to GI but is the most common cause of norovirus outbreaks worldwide.
- Rotavirus A: Highly contagious virus causing severe diarrhea, vomiting, fever, and abdominal pain, primarily in infants and young children.
Parasites
- Cryptosporidium: Causes cryptosporidiosis, leading to watery diarrhea, which can be particularly severe in immunocompromised individuals like those with autoimmune diseases.
- E. histolytica: Can result in lack of energy, weight loss, and GI issues, which can lead to dysentery with bloody diarrhea, and liver abscess if it spreads.
- Giardia: Causes giardiasis, characterized by symptoms such as foul-smelling diarrhea, stomach cramps, bloating, and nausea.
Helicobacter pylori (H. Pylori)
- H. Pylori: Known for causing ulcers in the stomach lining and increasing the risk of stomach cancer. This pathogen is also linked to chronic gastritis and peptic ulcers. Pro Knowledge: It can also slow stomach acid production, leading to fermentation and bubbling of food in the stomach, which can then lead to acid reflux.
- Virulence Factor, cagA: A protein associated with H. pylori, which increases its ability to cause damage and leads to more severe gastric diseases.
- Virulence Factor, vacA: A toxin produced by H. pylori that can lead to cell death in the stomach lining and contribute to ulcer formation.
Opportunistic Bacteria
- Citrobacter freundii: Can cause infections in the urinary tract and other parts of the body, may trigger symptoms in autoimmune conditions.
- Klebsiella pneumoniae: Known to cause pneumonia, it can also lead to other infections, particularly in individuals with weakened immune systems like autoimmune disease.
- Proteus: A group of bacteria that can cause urinary tract infections and may be linked to rheumatoid arthritis.
- Proteus mirabilis: This specific strain is also associated with urinary tract infections and could be implicated in kidney stone formation.
- Methanobacteriaceae: A family of bacteria that produces methane, which can negatively affect the overall balance of the gut microbiome.
- Fusobacterium: These bacteria are associated with several infections, including periodontal disease (like gum disease), and may have links to colorectal cancer.
- Desulfovibrio: Known for producing hydrogen sulfide, which can damage the gut lining and is associated with inflammatory bowel diseases (IBD).
Overgrowth Bacteria
- Morganella: Normally found in the human intestine, but if it overgrows, it can cause infections, particularly in the urinary tract.
- Pseudomonas: Known for its resistance to antibiotics and can cause various infections if it overgrows.
- Pseudomonas aeruginosa: A specific strain of Pseudomonas that can lead to respiratory system infections and is particularly problematic in hospitals.
- Staphylococcus: Can cause skin infections, pneumonia, and food poisoning when they overpopulate.
- Streptococcus: Can cause a wide range of health issues, from strep throat to more serious conditions like rheumatic fever if it grows unchecked.
Other Parasites
- Blastocystis hominis: Commonly found in the intestine; can sometimes cause digestive symptoms, but many people have no symptoms at all.
- Dientamoeba fragilis: May cause diarrhea, bloating, and stomach pain, although it is often found in people who have no digestive symptoms.
- Endolimax nana: Usually doesn’t cause problems but can be associated with gastrointestinal symptoms if they overgrow.
- Entamoeba coli: Not to be confused with E. coli bacteria, this parasite is typically harmless but can sometimes be a sign of poor sanitary conditions.
- Chilomastix mesnelli: Often found in the human digestive tract and usually doesn’t cause disease or symptoms but still is important in the overall microbiome.
- Pentatrichomonas hominis: Considered non-disease causing, but its presence may indicate exposure to other pathogens or poor hygiene.
Fungi/Yeast
- Candida albicans: This yeast can cause infections like thrush and yeast infections, particularly in individuals with weakened immune systems like autoimmunity.
- Candida: Similar to Candida albicans, these species can lead to various candidiasis infections, affecting skin, genitals, throat, and more.
- Geotrichum: Can cause a rare condition called geotrichosis, affecting the skin, bronchi, and lungs, mostly in immunocompromised individuals like in autoimmune disease.
- Microsporidium: These are microscopic parasites that can cause chronic diarrhea and wasting in people with compromised immune systems, such as those with AIDS and autoimmunity.
- Trichosporon: Typically harmless but can occasionally cause infections like white piedra, affecting the hair shafts, or more serious systemic infections if in the gut.
Additional GI Map Tests
- Secretory IgA (SIgA): This test measures the level of IgA antibodies in saliva and intestinal fluids, important for immune function in the gut.
- Anti-gliadin SIgA: Measures antibodies against gliadin, a component of gluten, to check for gluten sensitivity or celiac disease. A very common cause of bloating.
- Elastase-1: A test to evaluate pancreatic function / production.
- Eosinophil Activation Protein (EPX/EDN): This test looks for proteins released by eosinophils, a type of white blood cell, indicating allergic reactions or parasitic infections.
- Calprotectin: Measures a protein found in white blood cells in stool to detect inflammation in the intestines, useful in diagnosing conditions like IBD.
- b-Glucuronidase: An enzyme measurement that can indicate the general health of the gut flora and potential for toxin buildup. High levels can also cause hormone imbalances due to its ability to cause discarded hormones in the stool to be reabsorbed.
- Steatocrit: This test measures the amount of fat in stool to assess for conditions that affect fat absorption, like pancreatic insufficiency.
- Fecal Occult Blood: Tests for hidden (occult) blood in the stool, an early marker for colon cancer or other gastrointestinal disorders.
Antibiotic-Resistant Genes Test
This part of the GI Map stool test shows doctors if certain bacteria in your body are resistant to antibiotics. For example, H. Pylori, a bacteria that can live in the stomach and can slow stomach acid production, might not be stopped by some drugs if the test indicates “Positive” for resistance genes. Here are the 4 drugs that are used in the gene resistance testing:
- Amoxicillin
- Fluoroquinolones
- Clarithromycin
- Tetracycline
Here is a sample report for the GI Map’s antibiotic-resistant gene test. You can also review the sample of the full GI Map test results. It’s essential to review the preparations for the stool test.

Medical Review Board
Reviewed by Jeff Donohue M.D. from Body Logic and Brady Hurst DC, CCCN. Written by True Health Lab’s team of editorial health contributors.
Disclaimer: This information is for educational purposes only and not intended as medical advice. Consult your healthcare provider for personalized guidance.
Why Customers Trust True Health Labs – What People are saying
Also rated 4.6 out of 5 based on 3452 ShopperApproved reviews- See all TrueHealthLabs.com reviews.